Understanding Lyme Disease
Testing and Diagnosis for Lyme Disease
Key Points
-
Healthcare providers consider multiple factors when evaluating a patient for Lyme disease.
-
Laboratory diagnosis relies on a blood test that detects antibodies to the Lyme bacteria.
-
Antibodies can take several weeks to appear, so early tests may be negative.
-
The CDC recommends FDA-cleared antibody tests that follow a two-step process.
-
Some labs that do not accept private insurance may use tests not cleared by the FDA.
Diagnosis
When assessing a patient for Lyme disease, healthcare providers consider:
-
Signs and symptoms of Lyme disease
-
Likelihood of exposure to infected blacklegged ticks
-
Other possible illnesses that could cause similar symptoms
-
Laboratory test results, when indicated

Laboratory Testing
-
The CDC recommends FDA-cleared antibody tests for diagnosis.
-
Accuracy depends on timing:
-
Tests may be falsely negative in the first few weeks, especially if only a rash is present.
-
After 4–6 weeks, FDA-cleared tests have good sensitivity.
-
-
Once antibodies are present, tests usually remain positive for months to years, even after the bacteria are gone.
-
Warning: Some laboratories that do not accept private insurance may use non-FDA-cleared tests.
What a Diagnosis Means
-
Early treatment with antibiotics usually leads to rapid and complete recovery.
-
Later treatment is often still effective, but some patients may experience long-term nerve or joint damage.
-
Positive antibody tests can remain for years, but do not protect against re-infection.

About Tickborne Co-Infections
-
Blacklegged ticks can transmit multiple diseases. Having more than one is called a co-infection.
-
Anaplasmosis is the most common co-infection (up to 10% of Lyme patients).
-
Other possible co-infections:
-
Babesiosis (treated with different medications)
-
Powassan virus disease
-
Hard tick relapsing fever
-
-
Treatment overlap: Lyme and anaplasmosis are both treated with the same antibiotic.
-
If Lyme symptoms persist after antibiotics, your doctor may test for other infections.
-
Note: Bartonella and Mycoplasma are not proven to be spread by ticks. If diagnosed with these as “tick co-infections,” consider a second opinion.
Diagnosis of Lyme Disease
Clinical Diagnosis First
Because “classic” indicators of Lyme disease are not always present and commonly available laboratory tests lack sensitivity, diagnosis is primarily clinical. Providers must weigh:
-
Medical history
-
Presenting symptoms and signs
-
Risk of tick exposure
Tick exposure evidence:
-
In Europe, ~64% of Lyme patients recall a tick bite.
-
In the U.S., fewer than 30% recall a bite.
Erythema Migrans (EM) rash:
-
Considered pathognomonic (diagnostic hallmark) when seen in endemic areas.
-
Most EM rashes are solid pink-to-red lesions; fewer than 20% have the “bull’s-eye” appearance.
-
Often asymptomatic and easily overlooked unless carefully sought on exam.
-
Presence of EM should prompt immediate antibiotic therapy.
Differential diagnosis:
Patients presenting with flu-like illness, with or without rash, in endemic regions should be evaluated for Lyme disease. Other possibilities include:
-
STARI (Southern Tick-Associated Rash Illness)
-
Other tick-borne diseases
Limitations of Current Testing
Standard CDC two-tier strategy (since 1994):
-
ELISA (sensitive screening test).
-
IgM and IgG Western blots performed only if ELISA is positive or equivocal.
Problems:
-
Negative ELISA halts further testing → risk of missed diagnoses.
-
False negatives are common due to timing, disease stage, and confounders.
-
Seronegativity despite illness has been documented.
Western blot interpretation:
-
CDC criteria prioritize specificity (99%) → sensitivity is sacrificed.
-
Alternative band criteria may improve sensitivity.
-
Significant bands for Borrelia burgdorferi exposure: 23–25, 31, 34, 39, 83–93.
Emerging modalities:
-
Culture methods
-
T-cell activation testing
-
Antigen capture
-
Proteomic approaches
Bottom line: Lab tests can support but not definitively confirm or rule out Lyme disease.
Comprehensive Evaluation
Lyme is often called the “great imitator”. Symptoms may resemble:
-
Rheumatologic disorders
-
Neurologic disorders
-
Chronic fatigue syndrome (CFS)
-
Fibromyalgia
-
Other multi-system illnesses
Chronically ill Lyme patients may also harbor non-tick infections such as: EBV, CMV, HHV-6, Mycoplasma, Chlamydia pneumoniae, Parvovirus, Candida.
-
The interaction of Lyme with these opportunists remains poorly understood.
Diagnosis of Chronic Lyme Disease
For many, Lyme is acute. For others, it is chronic and persistent.
Common chronic symptoms:
-
Fatigue
-
Cognitive dysfunction (“brain fog”)
-
Headaches
-
Sleep disturbances
-
Migratory muscle/joint pain
-
Numbness and tingling
-
Neuropathic pain
-
Depression and anxiety
-
Musculoskeletal dysfunction
Evidence supporting chronic Lyme as distinct:
-
Symptoms differ from fibromyalgia, depression, and CFS (meta-analysis).
-
CSF protein profiles distinguish chronic Lyme from chronic fatigue syndrome.
Conclusion: As in early disease, comprehensive evaluation—clinical plus supportive testing—is essential.
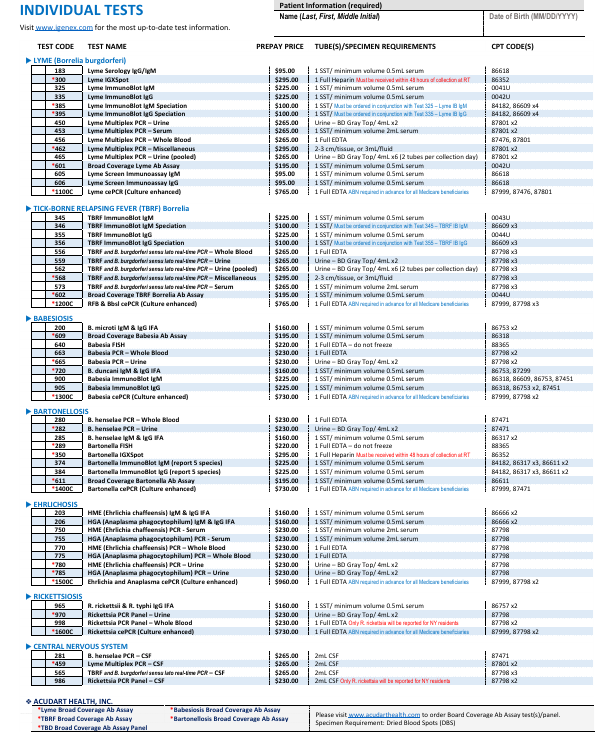
Testing Options Including Co-Infections for Quest
Lyme western blot
Lyme Elisa IGG/IGM
Babesia microti IGG/IGM
Babesia Ducani IGG/IGM
Bartonella Henselea AB IGG/IGM
Bartonella Quintana AB IGg/IGM
Ehrlichia Chaeensis IGG/IGM
Ehrlichia Equine IGG/IGM
Mycoplasma pneumonia AB IGG/IGM
Rickesttial Disease IGG/IGM
Q fever IGG/IGM phase I&II
Rocky Mountain Spotted Fever IGG/IGM
Brucella AB IGG/IGM Chlamydia Pneumonia IGG/IGA/IGM Tularemia IGG/IGM
Typhus IGG/IGM
CMV IGG/IGM
EBV IGG/IGM
Human herpes virus
IGG/IGMParvovirus AB IGG/IGM
Toxoplasma AB IGG/IGM
West Nile Virus AB IGG/IGM
Coxsackie virus IGG/IGM
Borrelia Myamotoi AB IGG/IGM ASO titer
Antidnase AB
TSH w reflex to free T4 CBC w di / platelets
CMP
CRP
ESR
Vitamin D serum

IGeneX VS other Labs
Broad, Multi-Pathogen Testing (Extensive Panel Offerings)
IGeneX offers an unusually comprehensive array of tests—not just for Lyme disease, but for a host of related tick‑borne infections including relapsing fever, Babesiosis, Bartonellosis, Rickettsiosis, Anaplasmosis, and Ehrlichiosis. They tailor both individual tests and broad panels that detect multiple co-infections simultaneously, more so than most other labs.
Advanced ImmunoBlot Technology with Recombinant Antigens
IGeneX has transitioned from the traditional Western blot to a proprietary ImmunoBlot that uses recombinant proteins.
This provides: Greater specificity: Recombinant proteins reduce ambiguous reactions.
Capability to detect multiple pathogens in one test, rather than the single‑pathogen focus of classic Western blots.
Multi-Strain Borrelia Detection
Unlike standard Lyme testing that targets a single strain of Borrelia burgdorferi, IGeneX includes proteins from several Borrelia strains or genospecies, enhancing detection across diverse geographic and genetic variants.
FDA-Cleared iDart™ ImmunoBlot Kits Featuring OspA and OspB
A landmark development—in mid-2025, IGeneX’s IgM and IgG ImmunoBlot kits (iDart™) received FDA clearance. These kits stand out because they:
Cover 26‑31 distinct antigen bands (IgM vs. IgG) representing multiple Borrelia species,
Include OspA (31 kDa) and OspB (34 kDa) antigens—no other FDA‑approved Lyme test has these, despite their high specificity.
This endorsement by the FDA is significant—they demonstrated both high sensitivity and specificity, confirming the robustness of IGeneX’s approach.
More Sensitive and Inclusive Interpretation Criteria
IGeneX moves away from the rigid CDC two‑tiered system (ELISA → Western blot, requiring specific band counts). Instead, their criteria allow for:
Positive results with just two or more Lyme‑specific bands, emphasizing the quality of the antigen over the number,
Detection across early, active, and late‑stage Lyme disease, without necessitating a first-tier screening test.
This translates to improved detection in patients who might only produce antibodies against a few key proteins—cases that traditional protocols often miss.
Deep Research & Clinical Focus
Founded in 1991 by Lyme‑disease pioneer Dr. Nick Harris and later joined by Dr. Jyotsna Shah, IGeneX has a long-standing commitment to improving diagnostic accuracy through:
In-house test development and ongoing scientific validation,
Educational outreach aimed at both clinicians and patients to improve understanding and interpretation of results.
| Feature | IGeneX Strength |
|---|---|
| Pathogen Coverage | Broad—many tick-borne diseases and co-infections |
| Test Type | Recombinant ImmunoBlot vs. traditional Western blot |
| Borrelia Strain Detection | Multiple strains/species versus one |
| FDA Clearance | Yes—iDart™ IgM & IgG ImmunoBlots (incl. OspA/OspB) |
| Interpretation Criteria | Sensitive—only two specific bands required |
| Clinical & Research Investment | Strong—test development and educational leadership |
IGeneX differentiates itself through
Enhanced sensitivity and specificity (thanks to recombinant protein technology, broader strain coverage, and OspA/OspB inclusion),
Comprehensive testing (including co-infections),
FDA backing for its ImmunoBlot kits—making it a go-to lab for clinicians seeking reliable testing for Lyme and associated tick-borne illnesses.
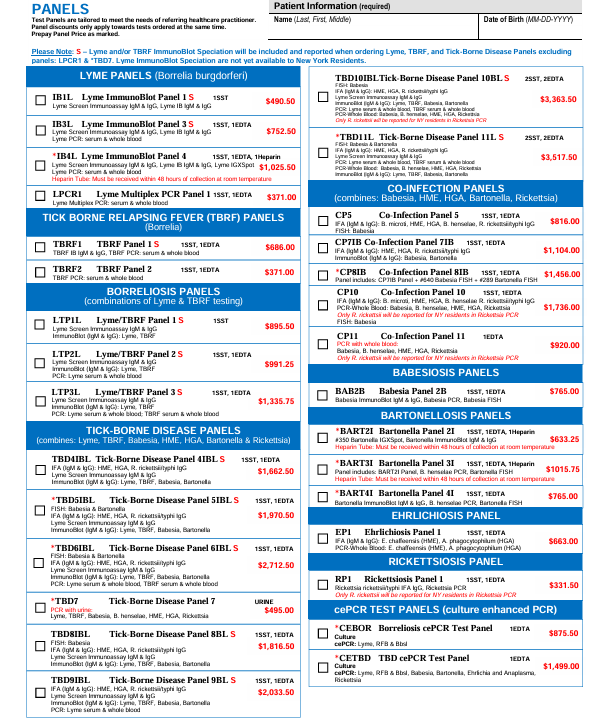
| Scenario / Feature | CDC Two-Tier (Quest / LabCorp / Hospital Labs) | IGeneX | Benefit of IGeneX |
|---|---|---|---|
| Early Lyme (0–6 weeks after bite) | ELISA often negative; Western blot requires multiple bands → misses early cases. | IgM ImmunoBlot detects early antibodies with broader antigen coverage; requires only 2 Lyme-specific bands. | Higher sensitivity → catches early cases before they spread. |
| Late / Disseminated Lyme | Optimized only for Borrelia burgdorferi (U.S. strain). | Includes recombinant proteins from multiple Borrelia species (B. afzelii, B. garinii, etc.). | Detects global strains, not just U.S. infections. |
| Unique Markers (OspA / OspB) | Excluded from FDA-cleared Western blot kits. | IGeneX ImmunoBlot includes OspA (31 kDa) & OspB (34 kDa). | Improves specificity (reduces false negatives). |
| Neurological / Atypical Cases | May test “negative” if antibody response is weak. | Can test multiple tick-borne pathogens (Babesia, Bartonella, etc.) alongside Lyme. | Identifies co-infections driving neuro/immune symptoms. |
| Co-Infections | Limited or no routine testing unless separately ordered; often less sensitive. | Panels include Babesia, Bartonella, Ehrlichia, Anaplasma, Relapsing Fever Borrelia. Uses antibody + PCR + FISH methods. | Comprehensive one-stop co-infection detection. |
| International Patients (Europe, Israel, Asia) | Lower accuracy outside U.S. strains. | Broad antigen pool covers multiple geographic strains. | Accurate diagnosis for global patients. |
| Interpretation Criteria | Must meet strict CDC definition (5/10 IgG bands or 2/3 IgM). “Indeterminate” often reported as negative. | Considers clinical relevance with fewer bands (2+). Reports detailed band info, not just “positive/negative.” | Provides clinically useful results instead of dismissive negatives. |
| FDA Status | FDA-cleared ELISA & Western blot kits. | 2025: FDA-cleared ImmunoBlot (iDart™) kits including OspA/OspB, multiple Borrelia strains. | FDA validation confirms accuracy + innovation. |
| Practicality for Doctors | Easy to order, covered by insurance, but low sensitivity. | Requires specialty lab ordering, sometimes out-of-pocket, but much higher diagnostic yield. | Better answers in complex or unresolved cases. |
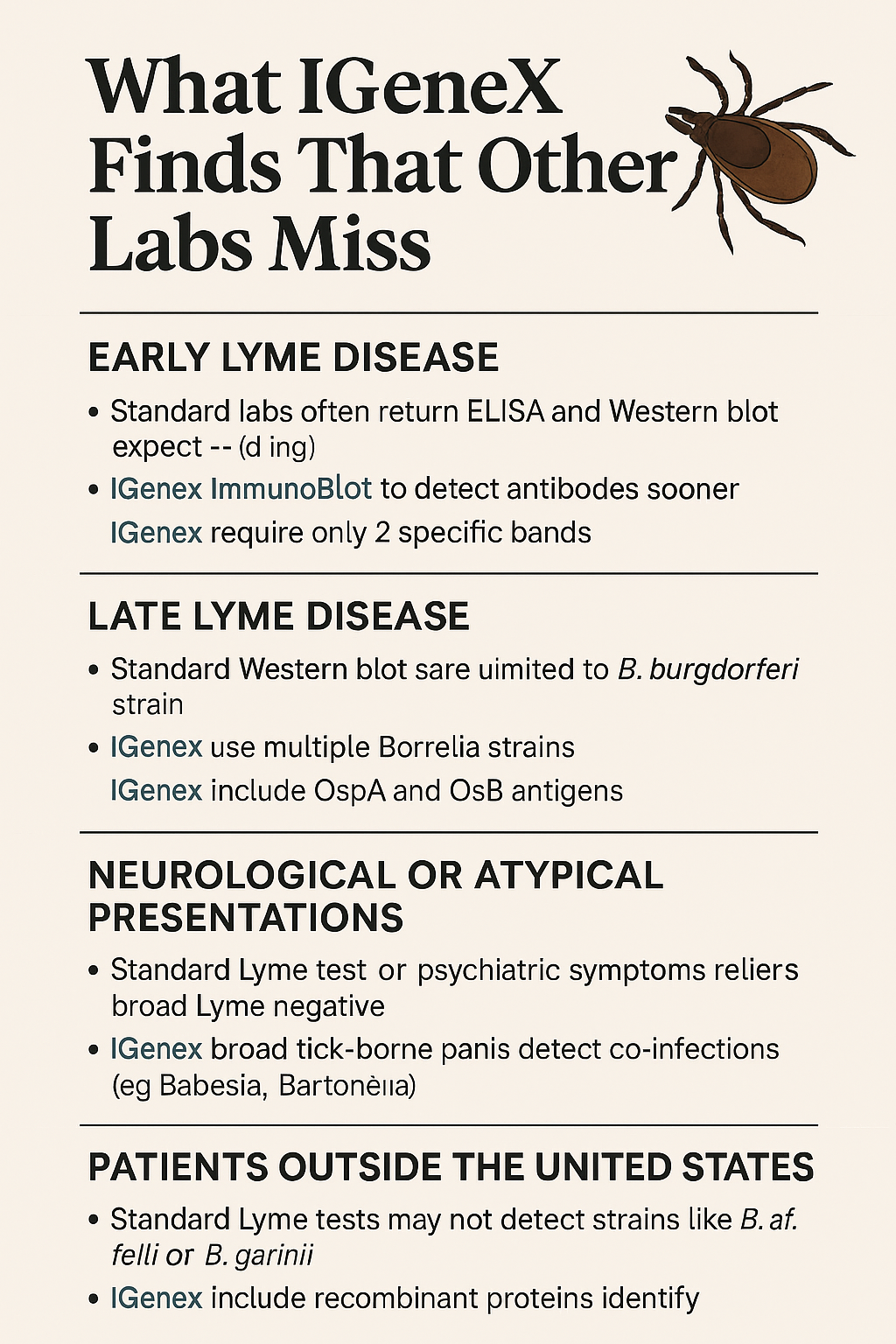
🔑 Key Takeaways
Quest/LabCorp are useful for ruling in clear, textbook cases but miss many early, late, or co-infected patients.
IGeneX is designed to find what standard labs miss — through broader strain coverage, more sensitive criteria, and inclusion of co-infections.
This matters most for patients who:
Have ongoing unexplained symptoms despite “negative” standard tests,
Live or traveled outside the U.S.,
Show neurological/psychiatric symptoms,
Or may have multiple infections at once.