Tick-Borne Disease Co-Infections
Why one tick bite can transmit more than one infection – and why testing beyond Lyme matters.
50%
of chronic
Lyme patients
report co-infections
30%
report two
or more
co-infections
”>5″
different pathogens
can be carried
by one tick
What are co-infections?
A co-infection is a simultaneous infection by two or more pathogens. In tick-borne illness, a single bite can transmit multiple pathogens at once. You can have any tick-borne pathogen without having Lyme.
Clinical takeaway:
Each suspected pathogen should be tested, diagnosed, and treated on its own. Treating Lyme alone won’t resolve co-infections.
Co-Infections
Overview
Black-legged ticks (Ixodes species) can transmit several pathogens in addition to Borrelia burgdorferi. Co-infections are an important consideration in patients with risk factors or persistent symptoms despite antibiotic treatment for Lyme disease.
-
Prevalence: The frequency of tick-borne co-infections in Lyme disease patients from endemic areas ranges from 4% to 45%.
-
Impact: Untreated co-infections increase morbidity and may interfere with the successful treatment of Lyme disease.
-
Testing Challenges: Laboratory tests vary in sensitivity and specificity, and often fail to account for strain differences among pathogens.
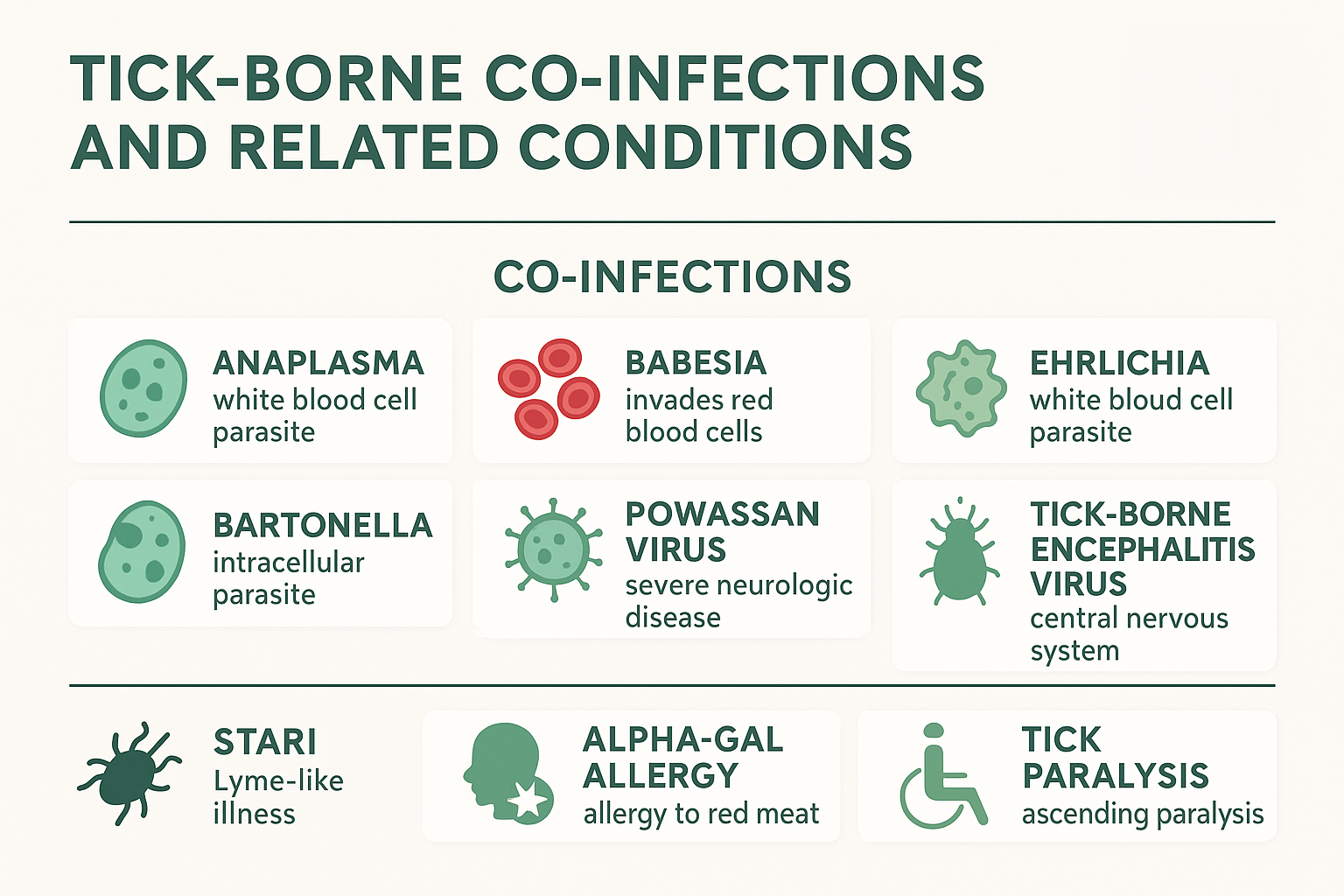
Commonly Encountered Co-Infections
-
Anaplasma
-
Intracellular white blood cell parasite
-
Symptoms: fever, headaches, body aches
-
Associated findings: leukopenia (low granulocytes), thrombocytopenia, elevated liver transaminases
-
-
Babesia
-
Malaria-like parasite (piroplasm) that invades red blood cells
-
Symptoms: fever, fatigue, chills, sweats, headaches, shortness of breath
-
Associated findings: anemia, elevated transaminases
-
-
Ehrlichia
-
White blood cell parasite, similar to Anaplasma
-
Clinical picture depends on species (different WBC types invaded)
-
Commonly associated with Lone Star ticks (Amblyomma americanum), though some strains are linked to Ixodes ticks
-
-
Bartonella
-
Intracellular parasite invading erythrocytes, endothelial, and other cells
-
Tick transmission: evidence increasing but not yet conclusive
-
Symptoms: fever, swollen lymph nodes, eye disorders, myocarditis, endocarditis, encephalopathy, musculoskeletal involvement
-
-
Powassan Virus
-
A flavivirus with two lineages; lineage II (deer tick virus) transmitted by Ixodes ticks
-
Symptoms: severe neurologic disease
-
Treatment: none currently available; fatalities documented
-
-
Tick-Borne Encephalitis Virus (TBEV)
-
Prominent in Europe and Asia
-
Affects the central nervous system
-
Treatment: none available
-
Prevention: vaccine used in parts of Europe (limited use in children due to adverse effects)
-
Selected Other Tick-Related Conditions
-
STARI (Southern Tick–Associated Rash Illness)
-
Lyme-like illness associated with Lone Star tick bites
-
Bacterial cause not yet established
-
Some evidence supports Lyme-like antibiotic treatment
-
Distribution: expanding beyond the southern and central US into the northeast
-
-
Alpha-Gal Allergy
-
IgE-mediated allergy to galactose-alpha-1,3-galactose (alpha-gal), a carbohydrate found in red meat
-
Triggered by Lone Star tick bites
-
Symptoms: delayed hypersensitivity reaction after eating red meat
-
Treatment: avoidance of red meat, allergy management
-
-
Tick Paralysis
-
Caused by neurotoxins in tick saliva during feeding
-
Symptoms: ascending paralysis
-
Treatment: removal of the tick (usually resolves symptoms)
-
Common co-infections (overview)
These are frequently reported alongside Lyme and other tick-borne diseases.
Babesia
Parasite • malaria-like illness
Night sweats Fatigue Air hunger
Often requires antiparasitic therapy.
Rickettsia rickettsii (RMSF)
Bacteria • Rocky Mountain Spotted Fever
High fever Rash Severe illness
Potentially deadly — urgent recognition and treatment are critical.
Bartonella
Bacteria • Cat Scratch Disease
Rashes/striae Foot pain Lymphadenopathy
May require prolonged antibiotics; presentation can be multisystemic.
Anaplasma
Bacteria • Anaplasmosis
Headache Chills Myalgia
Seen in multiple regions; consider in compatible epidemiology.
Ehrlichia
Bacteria • Ehrlichiosis
Fever Low WBC Liver involvement
Can be severe if untreated; prompt therapy is important.
Also consider
Other tick-borne pathogens
Powassan virus Borrelia miyamotoi (TBRF)
May present without Lyme; test if clinically suspected.
Why co-infections matter
| Implication | What it means |
|---|---|
| Separate testing | Each pathogen requires its own tests; a negative Lyme test doesn’t rule out other infections. |
| Targeted treatment | Therapies differ (e.g., antiparasitics vs. antibiotics vs. antivirals). Treating Lyme alone won’t cure co-infections. |
| Severity & recovery | Pathogen interactions may increase symptom burden and lengthen recovery times. |
| Risk awareness | Some infections (e.g., RMSF, Powassan) can be life-threatening if missed — timely diagnosis is essential. |
